More than 400,000 Americans have been diagnosed with Barrett’s esophagus, which causes the body to replace tissue lining the esophagus with cells that can become cancerous. But as many as 5 million people might have Barrett’s esophagus without knowing it, according to Stephen Meltzer, professor of medicine and oncology at The Johns Hopkins University’s Division of Gastroenterology and Hepatology.
There is no reliable and efficient way to screen everybody at risk for the disease, however, which is treatable if detected early enough.
“If you catch it in time, you’ll probably never die of esophageal cancer,” says Meltzer, noting Barrett’s esophagus can be detected in an upper endoscopy, but the procedure is not done regularly to screen all people at risk, unlike a colonoscopy.
“They could be walking around with a ticking time bomb,” he says.
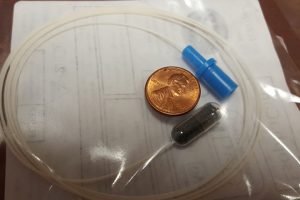
Meltzer, at Johns Hopkins’ GI Early Detection Biomarkers Laboratory, identified EsoBEE, a panel of four DNA biomarkers for the disease. To obtain genetic material for this biomarker test, his team uses a device known as the EsophaCap, a small capsule with a string attached that is swallowed by the patient. The capsule dissolves, leaving behind a 2-centimeter sponge that collects genetic material from the esophagus as it is retrieved by the string. The sponge is then tested at the lab for signs of cancer.
Meltzer published findings last month from a pilot study in the journal Clinical Cancer Research and is planning a larger study to verify the biomarkers hold up.
Ultimately, biomarker tests similar to EsoBEE might be used to screen for a myriad other upper GI illnesses, such as gastric cancer, without needing a doctor to perform the capsule procedure, Meltzer adds.
He is starting to develop EsoBEE as an available test, while other universities and private firms are developing similar technologies involving sponges.
“It’s a race,” he says. “The intense competition suggests that this is a realistic product and a viable, valuable idea.”