The following was originally published in Johns Hopkins Medicine’s Newsroom.
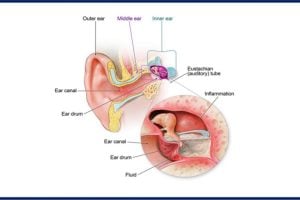
A child pulling his or her ear in pain typically results in a parent scheduling a doctor’s appointment to check for a medical problem. However, studies have consistently shown that it’s a coin toss whether or not a pediatrician or a non-specialist can correctly diagnose an ear infection.
“The ears are just a nice and easy thing about which to say, ‘This is why my child isn’t sleeping,’” says James Clark, M.B., B.Ch., B.A.O., assistant professor of otolaryngology – head and neck surgery at the Johns Hopkins University School of Medicine. “It’s a problem looking for an explanation.”
Incorrect diagnoses can be frustrating and time-consuming for parents, not to mention the ear, nose and throat doctors called in for a second opinion. Clark and Therese Canares, M.D., assistant professor in pediatric emergency medicine at the Johns Hopkins University School of Medicine, believe artificial intelligence (AI) could help better diagnose and manage ear infections, even remotely from a patient’s home. They are co-inventors of OtoPhoto, the world’s first smart otoscope, a device that takes images of the inner ear and uses machine learning to determine whether or not an infection exists.
OtoPhoto’s visuals are analyzed by a proprietary algorithm that makes the diagnosis. The images also can be shared with a specialist in real time during a telehealth appointment, an added benefit when many are avoiding office visits because of the enduring coronavirus pandemic.
“Even if there is an ear infection,” says Canares, “our hope is OtoPhoto enables them to get both the diagnosis and treatment at home, without getting exposed to COVID-19.”
OtoPhoto recently received $20,000 from the National Capital Consortium for Pediatric Device Innovation’s “Make Your Medical Device Pitch for Kids!” virtual competition. The development team also includes Mathias Unberath, Ph.D., an assistant professor in the Department of Computer Science at the Johns Hopkins Whiting School of Engineering; and John Rzasa, Ph.D., chief engineer at the Robert E. Fischell Institute for Biomedical Devices, within the A. James Clark School of Engineering at the University of Maryland, College Park.
The pitch award “validated that we were on to something, and that people outside our core team believe in us, too,” says Canares.
Along with developing a prototype thanks to a $300,000 grant from the Leon Lowenstein Foundation, the team has submitted a provisional patent application for its technology through Johns Hopkins Technology Ventures and is looking into forming a startup.
Canares and Clark have participated in Johns Hopkins’ I-Corps program, an immersive entrepreneurship learning experience developed by the National Science Foundation, as well as Hexcite, an early-stage medical software accelerator program hosted by the Johns Hopkins Medicine Technology Innovation Center.
Canares says the team hopes to have some very early efficacy data by the middle of 2021 as product development continues. Meanwhile, they have already started talking with parents of children with recurrent ear infections who are “head-over-heels for this idea,” she says.
“We’re starting to recognize that maybe there’s a need we can fill,” she says.