The following was originally published in Johns Hopkins Medicine’s Newsroom.
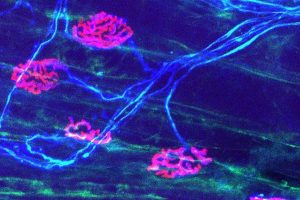
Peripheral nerves — the nerves outside the brain and spinal cord — have the capacity for regeneration, but the rate of renewal is so slow that many nerve injuries lead to incomplete recovery and permanent disability for patients. Johns Hopkins Medicine researchers have determined that macrophages — white blood cells that surround and kill microorganisms, remove dead tissues and stimulate the action of other immune system soldiers — can be modified to support and accelerate the regeneration of peripheral nerves in mice following injury.
In a study published Sept. 7, 2021, in the Journal of Clinical Investigation, Brett Morrison M.D., Ph.D., associate professor of neurology at the Johns Hopkins University School of Medicine; Mithilesh Kumar Jha, Ph.D., postdoctoral research fellow at Johns Hopkins; and colleagues investigated whether altering the metabolism of macrophages in mice would impact the recovery from nerve injury.
Using genetic manipulations on the macrophages, the researchers determined that removing a specific metabolic transporter (a protein that facilitates movement of metabolites across membranes) — monocarboxylate transporter 1 (MCT1) — delayed recovery from nerve injury. This was accompanied by alterations in several macrophage cellular functions, including the ability to collect foreign or dead cells, and to secrete specific cytokines (proteins produced by cells in the immune system) that communicate with other immune cells to coordinate the immune system’s overall response to injury.
The technology is available for licensing through Johns Hopkins Technology Ventures.
Of even greater clinical interest, say the researchers, was their discovery that increasing MCT1 in macrophages led to improved recovery following neve injury in mice.
“It was surprising how effective it was,” says Morrison. “We were able to accelerate the recovery from nerve injury by increasing MCT1. This opens up new avenues for potentially treating severe nerve injuries that can occur from traumas such as a motor vehicle accident or gunshot wounds.”
Jha says another exciting advance from the study was the demonstration that macrophages that were purified outside the body and intravenously injected into mice could impact nerve recovery.
“This finding could lead to a treatment for peripheral nerve injuries — for which no medical therapy currently exists — where a person could receive an injection of their own macrophages with upregulated levels [higher amounts from increased production] of MCT1,” he explains.
Morrison says he hopes his team’s research will one day be applied to human clinical trials.
“For the first time, we have demonstrated that manipulating macrophage metabolism can actually accelerate peripheral nerve regeneration,” says Morrison. “This is an exciting pathway that could potentially be manipulated in patients to treat peripheral nerve injuries.”