David Sidransky, M.D., calls the Pap smear one of the “greatest successes” in cancer screening.
“Every woman in the United States is supposed to be going for a regular Pap smear exam, and if they do, the chance of developing cervical cancer is very low,” says Sidransky, an expert in the molecular genetic detection of cancer and director of head and neck cancer research in the Department of Otolaryngology–Head and Neck Surgery at the Johns Hopkins University School of Medicine.
Despite the Pap smear’s effectiveness, however, there are geographic and racial disparities regarding who takes the test and what is an appropriate follow-up. Studies have shown that older women who did not receive the vaccine for the human papilloma virus (HPV, a known cause of cervical cancer) have a higher risk for developing cervical cancer, while Black women have a higher incidence of the disease and do more poorly after diagnosis. Moreover, in many Latino communities, the test isn’t widely accepted.
That’s why Sidransky has been working with former Johns Hopkins Medicine researcher Rafael Guerrero-Preston, Dr.P.H., M.P.H., on another way to identify women at greatest threat from cervical cancer — a home test they can do themselves. The self-administered screening tool can accurately identify a higher risk for future cervical cancer by finding methylated DNA segments.
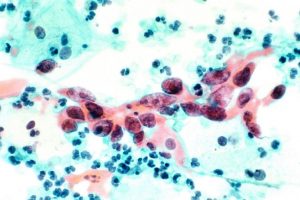
Higher levels of methylation — the addition of a methyl group (three hydrogen atoms bound to a carbon atom) to a DNA molecule — are associated with a greater likelihood that cervical cells will progress to a cancerous state.
“If someone tests positive and the early steps of cancer development are detected, we can treat it before it becomes invasive,” says Sidransky.
The new test involves a robust molecular process in which cells taken from a vaginal swab are used to detect both HPV and methylated DNA. While a Pap smear only analyzes a small sample of cells from a single spot on the cervix, Sidransky says the home test checks both the swab site and the surrounding region for cervical cancer’s early warning signals.
“Even if you miss the presence of a tumor, sampling the larger area enables you to diagnose a problem and better estimate the likelihood that it will progress to cancer,” he says.
Sidransky envisions that a woman could swab herself, mail the sample and get results back in less than two weeks, similar to the process for home colon cancer screening kits already in use.
“I think for us to succeed, ultimately the test must be able to be done in any lab,” he says. “The goal of this is to make this as low-cost and distributable as possible, including to lower income countries worldwide.”
The methylation test was licensed through Johns Hopkins Technology Ventures to LifeGene BioMarks, a Johns Hopkins spinoff company. Guerrero-Preston, the firm’s founder and chief scientific officer, worked in Sidranksy’s lab for a decade.
LifeGene BioMarks and Sidransky recently received two grants totaling more than $1.5 million through the U.S. Small Business Administration’s Small Business Innovation Research program. The grant funds will be used to first make the test more robust for improved cell sampling and then to enable clinicians to examine a larger number of samples for clinical validation.
“I think there is an excitement in terms of what this test could bring in advancing self–screening for cervical cancer and in bridging the disparity gaps that currently keep quality screening from all women,” Sidransky says.