Health care researchers estimate that in the future, half of all visits to primary care doctors will take place in the home with the help of rapidly expanding telecommunication technology, according to Rebecca Canino, administrative director of Johns Hopkins Telemedicine.
“Telemedicine is the use of technology to get care to you at the right place at the right time,” Canino said in the keynote address during Johns Hopkins Medicine’s Digital Health Day event.
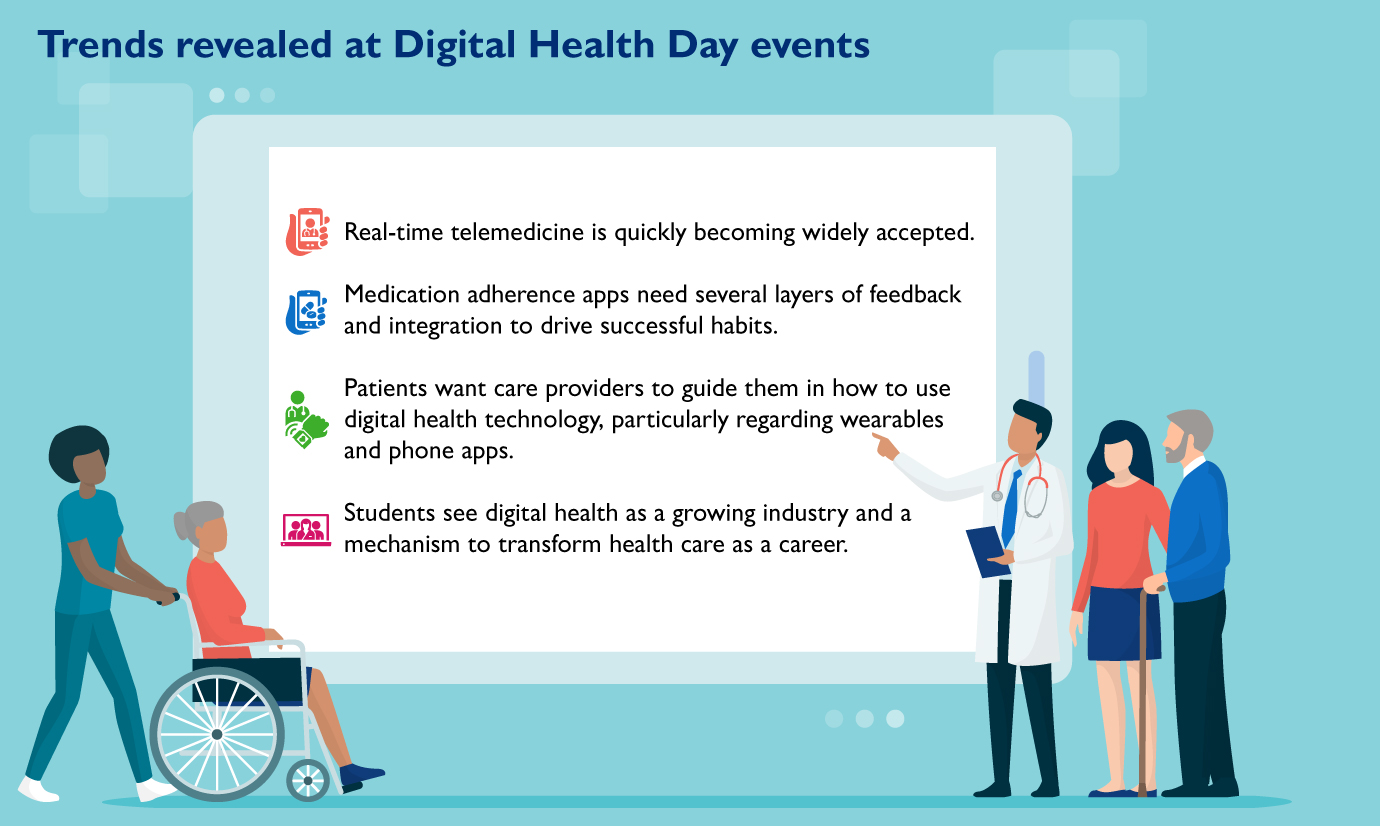
The third annual Digital Health Day, held Nov. 13 in Turner Concourse, attracted nearly 300 Johns Hopkins faculty and staff members, students and members of the local digital health entrepreneurial community. Digital Health Day is organized by the Technology Innovation Center, which collaborates with Johns Hopkins clinical researchers and care providers to improve patient care through medical software.
Representatives from Johns Hopkins Telemedicine, Johns Hopkins Technology Ventures and the Malone Center for Engineering in Healthcare helmed exhibitor booths, and so did vendors including Salesforce, Intel and Verizon, and spokespeople for startups such as b.well Connected Health and Oncospace.
Every half-hour, an exhibitor went on a demo stage to showcase cutting-edge technology that included 3D printers, telemedicine robots and virtual reality simulations.
“A lot of the future of medicine is being explored at Johns Hopkins,” said Paul Nagy, deputy director of the Technology Innovation Center, as he invited participants to consider how the digital health products and systems on display could aid their work.
For example, the b.well Connected Health app houses all of a user’s health-care-related information, including medical records, prescriptions, insurance and wellness programs.
Nagy said dozens of such projects are underway across the institution. “Doing digital health really is an experiment,” he said. “We’re here to bring this community together, to see different technology being applied in the (operating room) or at home, and to learn how (the technologies) might be able to help in the clinical setting.”
Michael Bowers, head of product development for Oncospace, demonstrated his company’s cloud-based software platform. It allows oncologists to use data from past patients to determine the most efficient and targeted treatment plans for new patients.
“The beauty of what we’re doing is that the data can be mined for predictive value in many different ways — we have lots of great ideas we’re exploring,” Bowers said.

Michael Bowers of Oncospace presents during Digital Health Day.
Oncospace is working toward 510(k) approval by the U.S. Food and Drug Administration, a premarket notification for medical devices.
Bowers says Digital Health Day offered opportunities to make contacts in the technical, financial and administrative worlds of health care.
“It was well organized, the pace of presentations was good and there was tremendous breadth of participation,” he says. “We could each tell our story in-depth and also hear what other people are doing.”
The number of Digital Health Day exhibitors grew from 26 in 2017 to 38 two years later, according to the Technology Innovation Center.
“What’s really been fun is growing a community,” Nagy says. “We’re seeing technology emerge from a shiny object to something that is moving the tipping point of improving care.”
Telemedicine at Johns Hopkins
Rebecca Canino, administrative director of Johns Hopkins Telemedicine, says studies show that 60% of millennials do not have, or necessarily want, a primary care doctor, while 44% prefer to go to retail clinics and are twice as likely as their parents to visit an urgent care center for medical issues.
Telemedicine fits this trend. The technology allows patients to chat with clinicians in real time through computers, smartphones or tablets. Some patients use telemedicine at home, while others participate through community centers, care facilities, schools or emergency departments equipped with telemedicine connections.
Johns Hopkins Telemedicine was founded in 2017 with the goals of improving access to and lowering the costs of care, as well as building sustainable programs and billing practices. It offers more than 60 programs in areas such as neurology, and more than 50 subservices for conditions including Parkinson’s disease and migraine headaches. It also provides chronic care management, remote observation and biometrics, according to Canino.
With access to the vital signs of patients at any hospital in the Johns Hopkins Health System, telemedicine nurses can coordinate care among providers and avoid unnecessary patient transfers. When a transfer is needed, the nurses can make the move happen as quickly as possible, saving the patient money on medical bills.
Telemedicine can also provide peace of mind, Canino says. For example, if a potential problem is spotted on a uterine scan halfway through a woman’s pregnancy, she might have to wait anxiously for a few days before she can receive a more in-depth scan and results. But if the sonogram is performed at an office working with Johns Hopkins Telemedicine, a maternal fetal medicine doctor can immediately order additional advanced scans and discuss the results via video conference minutes later.
“We are saving people money, time and anxiety while providing high quality care,” Canino says.